Page 810 - TNFlipTest
P. 810
NS12 Neurosurgery
CNS Tumours
Toronto Notes 2019
Table 8. Tumour Location: Etiology and Clinical Presentation
Epidemiology
Age <15 yr
Incidence: 2-5/100,000/yr 60% infratentorial
Age >15 yr
80% supratentorial
Clinical Presentation
Shared Features
(from elevated ICP)
Distinguishing Features
Supratentorial
Astrocytoma (all grades) (50%) Craniopharyngioma (2-5%)
Others: pineal region tumours, choroid plexus tumours, ganglioglioma, DNET
High grade astrocytoma (12-15%, e.g. GBM) Metastasis (15-30%, includes infratentorial) Meningioma (15-20%)
Low grade astrocytoma (8%)
Pituitary adenoma (5-8%) Oligodendroglioma (5%)
Other: colloid cyst, CNS lymphoma, dermoid/epidermoid cysts
Headache: usually worse in AM and made worse with straining, Nausea/Vomiting
Papilledema
Diplopia - CN VI palsy
Seizure: commonly the first symptom
Progressive neurological deficits (70%)
Frontal lobe: hemiparesis, dysphasia, personality changes, cognitive changes
Temporal lobe: auditory/olfactory hallucinations, memory deficits, contralateral superior quadrantanopsia
Mental Status Change: depression, apathy, confusion, lethargy
“Tumour TIA” – stroke like symptoms caused by
a) occlusion of vessel by tumour cells
b) hemorrhage
c) 2o to “steal phenomenon” - blood is shunted from
ischemic regions to non-ischemic regions Endocrine disturbance - with pituitary tumours (see Endocrinology, E36)
Infratentorial (Posterior Fossa)
Medulloblastoma (15-20%) Cerebellar astrocytoma (15%) Ependymoma (9%) Brainstem astrocytoma
Metastasis
Acoustic neuroma (schwannoma) (5-10%) Hemangioblastoma (2%)
Meningioma
coughing
Brainstem involvement: cranial nerve deficits and long tract signs Nausea/vomiting: compression on vagal nucleus/area postrema
Diplopia: direct compression CN VI Vertigo
Nystagmus
Truncal ataxia + titubation: cerebellar vermis lesions
Limb ataxia, dysmetria, intention tremor: cerebellar hemisphere lesions Obstructive hydrocephalus more common than supratentorial lesions
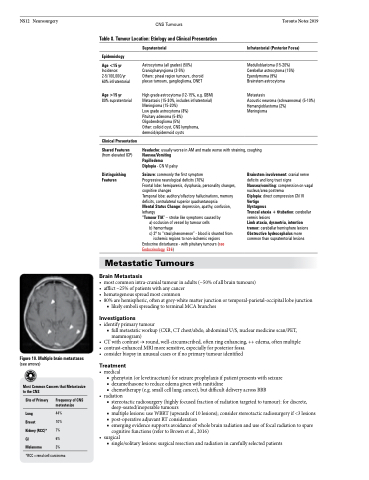
Figure 10. Multiple brain metastases
(see arrows)
Most Common Cancers that Metastasize to the CNS
• mostcommonintra-cranialtumourinadults(~50%ofallbraintumours)
• afflict~25%ofpatientswithanycancer
• hematogenousspreadmostcommon
• 80%arehemispheric,oftenatgrey-whitematterjunctionortemporal-parietal-occipitallobejunction
■ likely emboli spreading to terminal MCA branches
Investigations
• identifyprimarytumour
■ full metastatic workup (CXR, CT chest/abdo, abdominal U/S, nuclear medicine scan/PET,
mammogram)
• CTwithcontrast→round,well-circumscribed,oftenringenhancing,++edema,oftenmultiple • contrast-enhancedMRImoresensitive,especiallyforposteriorfossa
• considerbiopsyinunusualcasesorifnoprimarytumouridentified
Treatment
• medical
■ phenytoin (or levetiracetam) for seizure prophylaxis if patient presents with seizure ■ dexamethasone to reduce edema given with ranitidine
■ chemotherapy (e.g. small cell lung cancer), but difficult delivery across BBB
• radiation
■ stereotactic radiosurgery (highly focused fraction of radiation targeted to tumour): for discrete,
deep-seated/inoperable tumours
■ multiple lesions: use WBRT (upwards of 10 lesions); consider stereotactic radiosurgery if <3 lesions ■ post-operative adjuvant RT consideration
■ emerging evidence supports avoidance of whole brain radiation and use of focal radiation to spare
cognitive functions (refer to Brown et al., 2016) • surgical
■ single/solitary lesions: surgical resection and radiation in carefully selected patients
Metastatic Tumours
Brain Metastasis
Site of Primary
Lung
Breast
Kidney (RCC)* GI
Melanoma
Frequency of CNS metastasize
44% 10% 7% 6% 3%
*RCC=renal cell carcinoma