Page 811 - TNFlipTest
P. 811
Toronto Notes 2019 CNS Tumours
Prognosis
• mediansurvivalwithouttreatmentoncesymptomaticis~1mo,withoptimaltreatment6-9mo.The disease-specific Graded Prognostic Assessment (Ds-GPA) is a useful prognostic index. Prognosis varies depending on primary tumour type and extent of systemic tumour burden
Astrocytoma
• mostcommonprimaryintra-axialbraintumour,commonin4th-6thdecades
Neurosurgery NS13
5
1 2
Table 9. World Health Organization Astrocytoma Grading System
43
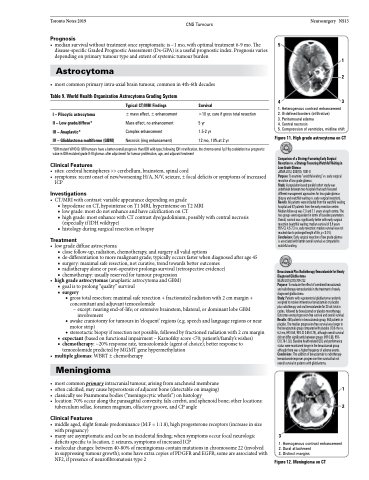
1. Heterogenous contrast enhancement 2. Ill-defined borders (infiltrative)
3. Peritumoural edema
4. Central necrosis
5. Compression of ventricles, midline shift
Figure 11. High grade astrocytoma on CT
Comparison of a Strategy Favouring Early Surgical Resection vs. a Strategy Favouring Watchful Waiting in Low-Grade Gliomas
JAMA 2012; 308(18): 1881-8
Purpose: To examine “watchful waiting” vs. early surgical resection of low grade gliomas.
Study: A population-based parallel cohort study was undertaken between two hospitals that each favoured different management approaches for low grade gliomas (biopsy and watchful waiting vs. early surgical resection). Results: 66 patients were included from the watchful waiting hospital and 87 patients from the early resection centre. Median follow-up was 7.0 and 7.1 years at each centre. The two groups were equivalent in terms of baseline parameters. Overall, survival was significantly better with early surgical resection (watchful waiting: median survival of 5.9 years 95% CI, 4.5-7.3 vs. early resection: median survival was not reached due to prolonged length of life, p<0.01). Conclusions: Early surgical resection of low grade-gliomas is associated with better overall survival as compared to watchful waiting.
Bevacizumab Plus Radiotherapy-Temozolamide for Newly Diagnosed Glioblastoma
NEJM2014;370:709-722
Purpose: To evaluate the effect of combined bevacizumab and radiotherapy-temozolamide in the treatment of newly diagnosed glioblastoma.
Study: Patients with supratentorial glioblastoma randomly assigned to receive intravenous bevacizumab or placebo plus radiotherapy and oral temozolamide for 30 wk total in cycles, followed by bevacizumab or placebo monotherapy. Outcomes were progression-free survival and overall survival. Results: 458 patients in bevacizumab group, 463 patients in placebo. The median progression-free survival was longer in the bevacizumab group compared with placebo (10.6 mo vs. 6.2 mo, HR 0.64, 95% CI 0.55-0.74), although overall survival did not differ significantly between groups (HR 0.88, 95%
CI 0.76-1.02). Baseline health-related QOL and performance status were maintained longer in the bevacizumab group although there was a higher frequency of adverse events. Conclusions: The addition of bevacizumab to radiotherapy- temozolamide improves progression-free survival but not overall survival in patients with glioblastoma.
1 2
3
1. Homogenous contrast enhancement 2. Dural attachment
3. Distinct margins
Figure 12. Meningioma on CT
I – Pilocytic astrocytoma
II – Low grade/diffuse*
III – Anaplastic*
IV – Glioblastoma multiforme (GBM)
Typical CT/MRI Findings
± mass effect, ± enhancement Mass effect, no enhancement Complex enhancement Necrosis (ring enhancement)
Survival
>10 yr, cure if gross total resection 5 yr
1.5-2 yr
12 mo, 10% at 2 yr
*IDH mutant WHO Gr II/III tumours have a better overall prognosis than IDH wild-type; following IDH stratification, the chromosomal 1p/19q codeletion has prognostic value in IDH mutated grade II–III gliomas after adjustment for tumour proliferation, age, and adjuvant treatment
Clinical Features
• sites:cerebralhemispheres>>cerebellum,brainstem,spinalcord
• symptoms:recentonsetofnew/worseningH/A,N/V,seizure,±focaldeficitsorsymptomsofincreased
ICP
Investigations
• CT/MRIwithcontrast:variableappearancedependingongrade
■ hypodense on CT, hypointense on T1 MRI, hyperintense on T2 MRI
■ low grade: most do not enhance and have calcification on CT
■ high grade: most enhance with CT contrast dye/gadolinium, possibly with central necrosis
(especially if IDH wildtype)
■ histology during surgical resection or biopsy
Treatment
• lowgradediffuseastrocytoma
■ close follow-up, radiation, chemotherapy, and surgery all valid options
■ de-differentiation to more malignant grade; typically occurs faster when diagnosed after age 45 ■ surgery: maximal safe resection, not curative, trend towards better outcomes
■ radiotherapy alone or post-operative prolongs survival (retrospective evidence)
■ chemotherapy: usually reserved for tumour progression
• high grade astrocytomas (anaplastic astrocytoma and GBM) ■ goal is to prolong “quality” survival
■ surgery
◆ gross total resection: maximal safe resection + fractionated radiation with 2 cm margin + concomitant and adjuvant temozolomide
– except: nearing end-of-life; or extensive brainstem, bilateral, or dominant lobe GBM involvement
◆ awake craniotomy for tumours in ‘eloquent’ regions (e.g. speech and language regions or near motor strip)
◆ stereotactic biopsy if resection not possible, followed by fractioned radiation with 2 cm margin ■ expectant(basedonfunctionalimpairment–Karnofskyscore<70;patient’s/family’swishes)
■ chemotherapy: ~20% response rate, temozolomide (agent of choice); better response to
temozolomide predicted by MGMT gene hypermethylation
• multiplegliomas:WBRT±chemotherapy
Meningioma
• mostcommonprimaryintracranialtumour,arisingfromarachnoidmembrane
• oftencalcified,maycausehyperostosisofadjacentbone(detectableonimaging)
• classicallyseePsammomabodies(“meningocyticwhorls”)onhistology
• location:70%occuralongtheparasagittalconvexity,falxcerebri,andsphenoidbone;otherlocations:
tuberculum sellae, foramen magnum, olfactory groove, and CP angle
Clinical Features
• middleaged,slightfemalepredominance(M:F=1:1.8),highprogesteronereceptors(increaseinsize with pregnancy)
• manyareasymptomaticandcanbeanincidentalfinding;whensymptomsoccurfocalneurologic deficits specific to location, ± seizures, symptoms of increased ICP
• molecular changes: between 40-80% of meningiomas contain mutations in chromosome 22 (involved in suppressing tumour growth); some have extra copies of PDGFR and EGFR; some are associated with NF2, if presence of neurofibromatosis type 2