Page 844 - TNFlipTest
P. 844
OB4 Obstetrics
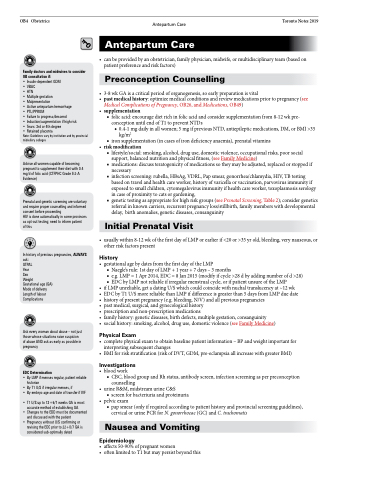
Family doctors and midwives to consider OB consultation if:
• Insulin-dependent GDM
• VBAC
• HTN
• Multiple gestation
• Malpresentation
• Active antepartum hemorrhage
• PTL/PPROM
• Failure to progress/descend
• Induction/augmentation if high risk
• Tears: 3rd or 4th degree
• Retained placenta
Note: Guidelines vary by institution and by provincial midwifery colleges
Advise all women capable of becoming pregnant to supplement their diet with 0.4 mg/d of folic acid (CTFPHC Grade II-2-A Evidence)
Prenatal and genetic screening are voluntary and require proper counselling and informed consent before proceeding
HIV is done automatically in some provinces as opt-out testing; need to inform patient
of this
In history of previous pregnancies, ALWAYS ask:
GTPAL
Year
Sex
Weight
Gestational age (GA) Mode of delivery Length of labour Complications
Ask every woman about abuse – not just those whose situations raise suspicion of abuse AND ask as early as possible in pregnancy
EDC Determination
• By LMP if menses regular, patient reliable historian
• By T1 U/S if irregular menses, if
• By embryo age and date of transfer if IVF
• T1 U/S up to 13+6/7 weeks GA is most accurate method of establishing GA
• Changes to the EDD must be documented and discussed with the patient
• Pregnancy without U/S confirming or revising the EDC prior to 22+0/7 GA is considered sub-optimally dated
•
• •
•
•
Antepartum Care Toronto Notes 2019 Antepartum Care
canbeprovidedbyanobstetrician,familyphysician,midwife,ormultidisciplinaryteam(basedon patient preference and risk factors)
Preconception Counselling
3-8wkGAisacriticalperiodoforganogenesis,soearlypreparationisvital pastmedicalhistory:optimizemedicalconditionsandreviewmedicationspriortopregnancy(see Medical Complications of Pregnancy, OB26, and Medications, OB49)
supplementation
■ folic acid: encourage diet rich in folic acid and consider supplementation from 8-12 wk pre- conception until end of T1 to prevent NTDs
◆ 0.4-1 mg daily in all women; 5 mg if previous NTD, antiepileptic medications, DM, or BMI >35 kg/m2
■ iron supplementation (in cases of iron deficiency anaemia), prenatal vitamins
riskmodification
■ lifestyle/social: smoking, alcohol, drug use, domestic violence, occupational risks, poor social support, balanced nutrition and physical fitness, (see Family Medicine)
■ medications: discuss teratogenicity of medications so they may be adjusted, replaced or stopped if necessary
■ infection screening: rubella, HBsAg, VDRL, Pap smear, gonorrhea/chlamydia, HIV, TB testing based on travel and health care worker, history of varicella or vaccination, parvovirus immunity if exposed to small children, cytomegalovirus immunity if health care worker, toxoplasmosis serology in case of proximity to cats or gardening,
■ genetic testing as appropriate for high risk groups (see Prenatal Screening, Table 2); consider genetics referral in known carriers, recurrent pregnancy loss/stillbirth, family members with developmental delay, birth anomalies, genetic diseases, consanguinity
Initial Prenatal Visit
usuallywithin8-12wkofthefirstdayofLMPorearlierif<20or>35yrold,bleeding,verynauseous,or other risk factors present
•
History
• gestational age by dates from the first day of the LMP
■ Naegle’srule:1stdayofLMP+1year+7days–3months
■ e.g. LMP = 1 Apr 2014, EDC = 8 Jan 2015 (modify if cycle >28 d by adding number of d >28) ■ EDC by LMP not reliable if irregular menstrual cycle, or if patient unsure of the LMP
• ifLMPunreliable,getadatingU/Swhichcouldcoincidewithnuchaltranslucencyat~12wk
• EDC by T1 U/S more reliable than LMP if difference is greater than 5 days from LMP due date • history of present pregnancy (e.g. bleeding, N/V) and all previous pregnancies
• pastmedical,surgical,andgynecologicalhistory
• prescriptionandnon-prescriptionmedications
• familyhistory:geneticdiseases,birthdefects,multiplegestation,consanguinity
• socialhistory:smoking,alcohol,druguse,domesticviolence(seeFamilyMedicine)
Physical Exam
• completephysicalexamtoobtainbaselinepatientinformation–BPandweightimportantfor interpreting subsequent changes
• BMIforriskstratification(riskofDVT,GDM,pre-eclampsiaallincreasewithgreaterBMI)
Investigations
• bloodwork
■ CBC, blood group and Rh status, antibody screen, infection screening as per preconception
counselling
• urineR&M,midstreamurineC&S
■ screen for bacteriuria and proteinuria • pelvicexam
■ pap smear (only if required according to patient history and provincial screening guidelines), cervical or urine PCR for N. gonorrhoeae (GC) and C. trachomatis
Nausea and Vomiting
Epidemiology
• affects50-90%ofpregnantwomen
• oftenlimitedtoT1butmaypersistbeyondthis