Page 834 - TNFlipTest
P. 834
NS36 Neurosurgery
Pediatric Neurosurgery
Toronto Notes 2019
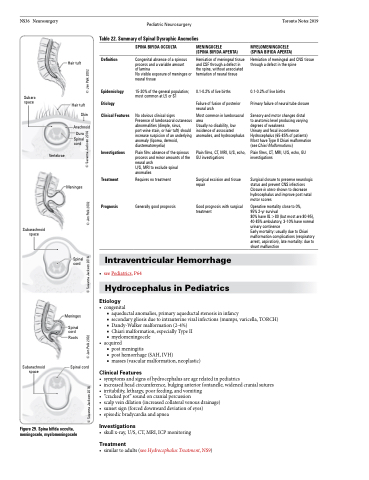
Table 22. Summary of Spinal Dysraphic Anomolies
Subarachnoid space
Hair tuft
Hair tuft Skin
Arachnoid Dura
Spinal cord
Meninges
Spinal cord
Meninges
Spinal cord
Roots
Spinal cord
Definition
Epidemiology Etiology
Clinical Features
Investigations
Treatment
Prognosis
SPINA BIFIDA OCCULTA
Congenital absence of a spinous process and a variable amount
of lamina
No visible exposure of meninges or neural tissue
15-20% of the general population; most common at L5 or S1
No obvious clinical signs
Presence of lumbosacral cutaneous abnormalities (dimple, sinus, port-wine stain, or hair tuft) should increase suspicion of an underlying anomaly (lipoma, dermoid, diastematomyelia)
Plain film: absence of the spinous process and minor amounts of the neural arch
U/S, MRI to exclude spinal anomalies
Requires no treatment
Generally good prognosis
MENINGOCELE
(SPINA BIFIDA APERTA)
Herniation of meningeal tissue and CSF through a defect in the spine, without associated herniation of neural tissue
0.1-0.2% of live births
Failure of fusion of posterior neural arch
Most common in lumbosacral area
Usually no disability, low incidence of associated anomalies, and hydrocephalus
Plain films, CT, MRI, U/S, echo, GU investigations
Surgical excision and tissue repair
Good prognosis with surgical treatment
MYELOMENINGOCELE (SPINA BIFIDA APERTA)
Herniation of meningeal and CNS tissue through a defect in the spine
0.1-0.2% of live births
Primary failure of neural tube closure
Sensory and motor changes distal
to anatomic level producing varying degrees of weakness
Urinary and fecal incontinence Hydrocephalus (65-85% of patients) Most have Type II Chiari malformation (see Chiari Malformations)
Plain films, CT, MRI, U/S, echo, GU investigations
Surgical closure to preserve neurologic status and prevent CNS infections Closure in utero shown to decrease hydrocephalus and improve post natal motor scores
Operative mortality close to 0%,
95% 2-yr survival
80% have IQ >80 (but most are 80-95), 40-85% ambulatory, 3-10% have normal urinary continence
Early mortality: usually due to Chiari malformation complications (respiratory arrest, aspiration), late mortality: due to shunt malfunction
Vertebrae
Subarachnoid space
Intraventricular Hemorrhage
• seePediatrics,P64
Hydrocephalus in Pediatrics
Etiology
Subarachnoid space
• congenital
■ aqueductal anomalies, primary aqueductal stenosis in infancy
■ secondary gliosis due to intrauterine viral infections (mumps, varicella, TORCH) ■ Dandy-Walker malformation (2-4%)
■ Chiari malformation, especially Type II
■ myelomeningocele
• acquired
■ post meningitis
■ post hemorrhage (SAH, IVH)
■ masses (vascular malformation, neoplastic)
Clinical Features
• symptomsandsignsofhydrocephalusareagerelatedinpediatrics
• increasedheadcircumference,bulginganteriorfontanelle,widenedcranialsutures • irritability,lethargy,poorfeeding,andvomiting
• “crackedpot”soundoncranialpercussion
• scalpveindilation(increasedcollateralvenousdrainage)
• sunsetsign(forceddownwarddeviationofeyes)
• episodicbradycardiaandapnea
Investigations
• skullx-ray,U/S,CT,MRI,ICPmonitoring
Treatment
• similartoadults(seeHydrocephalusTreatment,NS9)
Figure 29. Spina bifida occulta, meningocele, myelomeningocele
© Savanna Jackson 2016
© Jen Polk 2002 ©SSaavvaannnaaJJaacckkssoonn22001166 © Jen Polk 2002 © Savanna Jackson 2016 © Jen Polk 2002