Page 821 - TNFlipTest
P. 821
Toronto Notes 2019 Vascular Malformations
Prognosis
• 30-dmortalityrate44%,mostlyduetocerebralherniation • rebleedrate2-6%,higherifHTNpoorlycontrolled
Vascular Malformations
Types
• arteriovenousmalformations(AVMs)
• cavernousmalformations(cavernomas,cavernoushemangiomas/angiomas)
• venousangioma
• capillarytelangiectasias
• arteriovenousfistula(AVF)(carotid-cavernousfistula,duralAVF,veinofGalenaneurysm) • “angiographicallyoccultvascularmalformations”(anytype,10%ofmalformations)
Arteriovenous Malformations, Cavernous Malformations, and Dural Fistulas
Table 13. Comparison of Pathoetiology, Clinical Presentation, and Treatment of Arteriovenous Malformations, Cavernous Malformations, and Dural Fistula’s
Neurosurgery NS23
Definition
Epidemiology
Clinical Features
Investigations
Treatment
Prognosis
Arteriovenous Malformation
Tangle of abnormal vessels/arteriovenous shunts, with no intervening capillary beds or brain parenchyma; usually congenital
Prevalence ~0.14%, M:F = 2:1, average age at diagnosis = 33 yr
15-20% of patients with hereditary hemorrhagic telengiectasia (Osler-Weber-Rendu syndrome) will have cerebral AVMs
Hemorrhage (40-60%): small AVMs are more likely to bleed due to direct high pressure AV connections
Seizures (50%): more common with larger AVMs Mass effect
Focal neurological signs secondary to ischemia (high flow → “steal phenomena”)
Localized headache, increased ICP
Bruit (especially with dural AVMs)
May be asymptomatic (“silent”)
MRI (flow void), MRA
Angiography (7% will also have one or more associated aneurysms)
Decreases risk of future hemorrhage and seizure Surgical excision is treatment of choice even in Spetzler-Martin Grades I – II with general good health
SRS (stereotactic radiosurgery) is preferred for small (<3 cm) or very deep lesions Endovascular embolization (glue, balloon) can be curative (5%) or used as adjuvant to surgery or SRS in larger lesions
Conservative (e.g. palliative embolization, seizure control if necessary)
10% mortality, 30-50% morbidity (serious neurological deficit) per bleed
Risk of major bleed in untreated AVMs: 2-4%/yr
Cavernous Malformations
Benign vascular hamartoma consisting of irregular sinusoidal vascular channels located within the brain without intervening neural tissue or associated large arteries/veins
Several genes now described: CCM1, CCM2, CCM3
Prevalence of 0.1-0.2%, both sporadic and hereditary forms described
Seizures (60%), progressive neurological deficit (50%), hemorrhage (20%), H/A
Often an incidental finding Hemorrhage risk less than AVM, usually minor bleeds
T2WI MRI (non-enhancing) Gradient echo sequencing (best for diagnosis)
Surgical excision:
Only appropriate for symptomatic lesions that
are surgically accessible (supratentorial lesions are less likely to bleed than infratentorial lesions)
Dural Fistulas
Fistula’s connecting dural arteries to dural veins or the dural sinus Frequently described to occur
at the transverse and cavernous sinuses, but can be found at every cranial dural sinus
Hypothesized to be related
to venous sinus thrombosis formation, and subsequent microvascular shunt formation within the dura between arteries and veins
Unknown true incidence Constitute 10-15% of all intracranial vascular abnormalities
Asymptomatic, pulsatile tinnitus if involving sigmoid or transverse sinuses, bruits, headache Carotid cavernous involvement classically produces proptosis, chemosis, and bruits
Symptoms of SAH, SDH, or ICH
Non-enhanced CT to r/o hemorrhage
MRI; however, this does not demonstrate the arterial supply to the fistula
Angiography remains the gold standard
Approach is dependent on size, location and symptoms, and includes:
Conservative treatment Neuroradiological endovascular interventions
Radiation therapy
Surgery
Combination of the above
8.1% annual risk of hemorrhage 6.9% annual risk for non- hemorrhagic neurological deficit 10.4% mortality rate
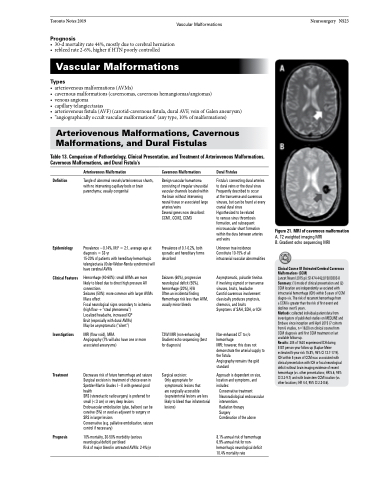
Figure 21. MRI of cavernous malformation
A. T2 weighted imaging MRI
B. Gradient echo sequencing MRI
Clinical Course Of Untreated Cerebral Cavernous Malformations (CCM)
Lancet Neurol 2015 pii: S1474-4422(15)00303-8 Summary: (1) mode of clinical presentation and (2) CCM location are independently associated with intracranial hemorrhage (ICH) within 5 years of CCM diagno-sis. The risk of recurrent hemorrhage from
a CCM is greater than the risk of first event and declines over 5 years.
Methods: collected individual patient data from investigators of published studies on MEDLINE and Embase since inception until April 2015 (7 cohorts from 6 studies, n=1620) on clinical course from CCM diagnosis until first CCM treatment or last available follow-up.
Results: 204 of 1620 experienced ICH during 5187 person-year follow-up (Kaplan-Meier estimated 5-year risk 15.8%, 95% CI 13.7-17.9). ICH within 5 years of CCM was associated with clinical presentation with ICH or focal neurological deficit without brain imaging evidence of recent hemorrhage (vs. other presentations; HR 5.6, 95% CI 3.2-9.7) and with brainstem CCM location (vs. other locations; HR 4.4, 95% CI 2.3-8.6).