Page 875 - TNFlipTest
P. 875
Toronto Notes 2019
Normal Labour and Delivery
Obstetrics OB35
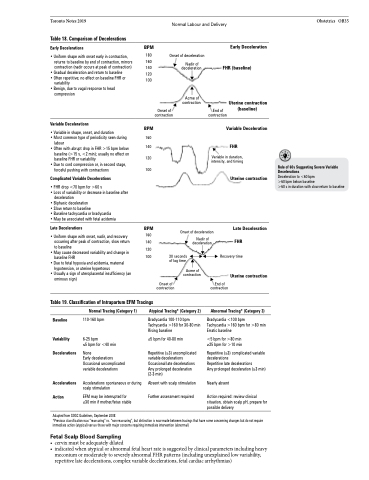
Table 18. Comparison of Decelerations
Early Decelerations
BPM
180
120 100
BPM
Early Deceleration FHR (baseline)
• Uniform shape with onset early in contraction,
returns to baseline by end of contraction, mirrors 160 contraction (nadir occurs at peak of contraction) 140
Onset of deceleration
• Gradual deceleration and return to baseline • Often repetitive; no effect on baseline FHR or
variability
• Benign, due to vagal response to head
compression
Variable Decelerations
Nadir of deceleration
Acme of contraction
Uterine contraction (baseline)
labour
• Often with abrupt drop in FHR >15 bpm below
baseline (>15 s, <2 min); usually no effect on
140
Onset of contraction
End of contraction
• Variable in shape, onset, and duration
• Most common type of periodicity seen during 160
Variable Deceleration
FHR
Variable in duration, intensity, and timing
Uterine contraction
Late Deceleration
FHR
Recovery time
Uterine contraction
Abnormal Tracing* (Category 3)
Bradycardia <100 bpm
Tachycardia >160 bpm for >80 min Erratic baseline
<5 bpm for >80 min ≥25 bpm for >10 min
Repetitive (≥3) complicated variable decelerations
Repetitive late decelerations
Any prolonged deceleration (≥3 min)
Nearly absent
Action required: review clinical situation, obtain scalp pH, prepare for possible delivery
baseline FHR or variability 120 • Due to cord compression or, in second stage,
forceful pushing with contractions 100
Rule of 60s Suggesting Severe Variable Decelerations
Deceleration to <60 bpm
>60 bpm below baseline
>60 s in duration with slow return to baseline
Complicated Variable Decelerations
• FHR drop <70 bpm for >60 s
• Loss of variability or decrease in baseline after
deceleration
• Biphasic deceleration
• Slow return to baseline
• Baseline tachycardia or bradycardia
• May be associated with fetal acidemia
Late Decelerations
• Uniform shape with onset, nadir, and recovery occurring after peak of contraction, slow return to baseline
• May cause decreased variability and change in baseline FHR
• Due to fetal hypoxia and acidemia, maternal hypotension, or uterine hypertonus
• Usually a sign of uteroplacental insufficiency (an ominous sign)
BPM
160 140 120 100
Onset of deceleration
Nadir of deceleration
30 seconds of lag time
Acme of contraction
Onset of contraction
End of contraction
Table 19. Classification of Intrapartum EFM Tracings
Baseline
Variability Decelerations
Accelerations Action
Normal Tracing (Category 1)
110-160 bpm 6-25 bpm
≤5 bpm for <40 min
None
Early decelerations Occasional uncomplicated variable decelerations
Accelerations spontaneous or during scalp stimulation
EFM may be interrupted for ≤30 min if mother/fetus stable
Atypical Tracing* (Category 2)
Bradycardia 100-110 bpm Tachycardia >160 for 30-80 min Rising baseline
≤5 bpm for 40-80 min Repetitive (≥3) uncomplicated
variable decelerations Occasional late decelerations Any prolonged deceleration (2-3 min)
Absent with scalp stimulation Further assessment required
Adapted from SOGC Guidelines, September 2008
*Previous classification was “reassuring” vs. “non-reassuring”, but distinction is now made between tracings that have some concerning changes but do not require immediate action (atypical) versus those with major concerns requiring immediate intervention (abnormal)
Fetal Scalp Blood Sampling
• cervixmustbeadequatelydilated
• indicatedwhenatypicalorabnormalfetalheartrateissuggestedbyclinicalparametersincludingheavy
meconium or moderately to severely abnormal FHR patterns (including unexplained low variability, repetitive late decelerations, complex variable decelerations, fetal cardiac arrhythmias)