Page 861 - TNFlipTest
P. 861
Toronto Notes 2019 Multi-Fetal Gestation and Malpresentation Obstetrics OB21 Polyhydramnios/Oligohydramnios
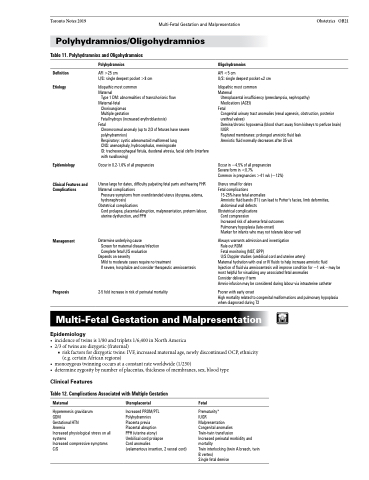
Table 11. Polyhydramnios and Oligohydramnios
Definition Etiology
Polyhydramnios
AFI >25 cm
U/S: single deepest pocket >8 cm
Idiopathic most common Maternal
Type 1 DM: abnormalities of transchorionic flow Maternal-fetal
Chorioangiomas
Multiple gestation
Fetal hydrops (increased erythroblastosis)
Fetal
Chromosomal anomaly (up to 2/3 of fetuses have severe polyhydramnios)
Respiratory: cystic adenomatoid malformed lung
CNS: anencephaly, hydrocephalus, meningocele
GI: tracheoesophageal fistula, duodenal atresia, facial clefts (interfere with swallowing)
Occur in 0.2-1.6% of all pregnancies
Uterus large for dates, difficulty palpating fetal parts and hearing FHR Maternal complications
Pressure symptoms from overdistended uterus (dyspnea, edema,
hydronephrosis) Obstetrical complications
Cord prolapse, placental abruption, malpresentation, preterm labour, uterine dysfunction, and PPH
Determine underlying cause
Screen for maternal disease/infection Complete fetal U/S evaluation
Depends on severity
Mild to moderate cases require no treatment
If severe, hospitalize and consider therapeutic amniocentesis
2-5 fold increase in risk of perinatal mortality
Oligohydramnios
AFI <5 cm
U/S: single deepest pocket ≤2 cm
Idiopathic most common Maternal
Uteroplacental insufficiency (preeclampsia, nephropathy)
Medications (ACEI) Fetal
Congenital urinary tract anomalies (renal agenesis, obstruction, posterior urethral valves)
Demise/chronic hypoxemia (blood shunt away from kidneys to perfuse brain) IUGR
Ruptured membranes: prolonged amniotic fluid leak Amniotic fluid normally decreases after 35 wk
Occur in ~4.5% of all pregnancies Severe form in <0.7%
Common in pregnancies >41 wk (~12%)
Uterus small for dates Fetal complications
15-25% have fetal anomalies
Amniotic fluid bands (T1) can lead to Potter’s facies, limb deformities, abdominal wall defects
Obstetrical complications
Cord compression
Increased risk of adverse fetal outcomes Pulmonary hypoplasia (late-onset)
Marker for infants who may not tolerate labour well
Always warrants admission and investigation
Rule out ROM
Fetal monitoring (NST, BPP)
U/S Doppler studies (umbilical cord and uterine artery)
Maternal hydration with oral or IV fluids to help increase amniotic fluid Injection of fluid via amniocentesis will improve condition for ~1 wk – may be most helpful for visualizing any associated fetal anomalies
Consider delivery if term
Amnio-infusion may be considered during labour via intrauterine catheter
Poorer with early onset
High mortality related to congenital malformations and pulmonary hypoplasia when diagnosed during T2
Epidemiology
Clinical Features and Complications
Management
Prognosis
Multi-Fetal Gestation and Malpresentation
Epidemiology
• incidenceoftwinsis1/80andtriplets1/6,400inNorthAmerica • 2/3oftwinsaredizygotic(fraternal)
■ risk factors for dizygotic twins: IVF, increased maternal age, newly discontinued OCP, ethnicity (e.g. certain African regions)
• monozygoustwinningoccursataconstantrateworldwide(1/250)
• determinezygositybynumberofplacentas,thicknessofmembranes,sex,bloodtype
Clinical Features
Table 12. Complications Associated with Multiple Gestation
Maternal
Hyperemesis gravidarum GDM
Gestational HTN
Anemia
Increased physiological stress on all systems
Increased compressive symptoms C/S
Uteroplacental
Increased PROM/PTL
Polyhydramnios
Placenta previa
Placental abruption
PPH (uterine atony)
Umbilical cord prolapse
Cord anomalies
(velamentous insertion, 2 vessel cord)
Fetal
Prematurity*
IUGR
Malpresentation
Congenital anomalies
Twin-twin transfusion
Increased perinatal morbidity and mortality
Twin interlocking (twin A breech, twin B vertex)
Single fetal demise