Page 858 - TNFlipTest
P. 858
OB18 Obstetrics
Obstetrical Complications
Toronto Notes 2019
Investigations
• sterilespeculumexam(avoidintroductionofinfection)
■ pooling of fluid in the posterior fornix
■ cascading: fluid leaking out of cervix with cough/valsalva
• nitrazine(basicamnioticfluidturnsnitrazinepaperblue)
■ low specificity as it can also be positive with blood, urine, or semen
• ferning:saltinamnioticfluidevaporates,givingamnioticfluidtheappearanceoffernsonmicroscopy • U/Storuleoutfetalanomalies;assessGA,presentation,andBPP
Management
• admit for expectant management and monitor vitals q4h, daily NST, WBC count, increased surveillance • avoidintroducinginfectionbyminimizingexaminations
■ consider administration of betamethasone valerate (Celestone®) to accelerate maturity if <34 wk and up to 36+6 weeks if no evidence of infection
■ consider tocolysis for 48 h to permit administration of steroids if PPROM induces labour
• screenwomenforUTIs,STIs,GBSinfectionandtreatwithappropriateantibioticsifpositive(treatGBS
at time of labour)
• ifnotinlabourorlabournotindicated,considerantibiotics:penicillinsormacrolideantibioticsarethe
antibiotics of choice
• deliver urgently if evidence of fetal distress and/or chorioamnionitis
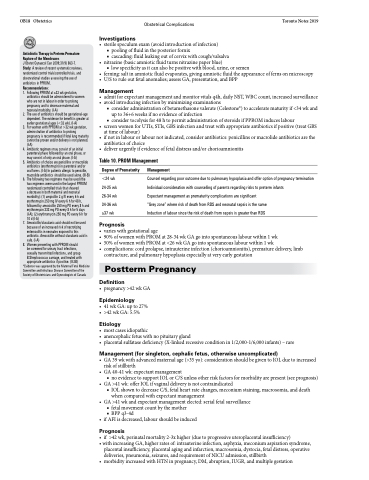
Table 10. PROM Management
Antiobiotic Therapy in Preterm Premature Rupture of the Membranes
J Obstet Gynaecol Can 2009;31(9) 863-7. Study: A review of recent systematic reviews, randomized control trials/controlled trials, and observational studies assessing the use of antibiotics in PPROM.
Recommendations:
1. FollowingPPROMat≤32wkgestation,
antibiotics should be administered to women who are not in labour in order to prolong pregnancy and to decrease maternal and neonatal morbidity. (I-A)
2. The use of antibiotics should be gestational-age dependent. The evidence for benefit is greater at earlier gestational ages (<32 wk). (I-A)
3. ForwomenwithPPROMat>32wkgestation, administration of antibiotics to prolong pregnancy is recommended if fetal lung maturity cannot be proven and/or delivery is not planned. (I-A)
4. Antibiotic regimens may consist of an initial parenteral phase followed by an oral phase, or may consist of only an oral phase. (I-A)
5. Antibiotics of choice are penicillins or macrolide antibiotics (erythromycin) in parenteral and/or oral forms. (I-A) In patients allergic to penicillin, macrolide antibiotics should be used alone. (III-B)
6. The following two regimens may be used (the two regimens were used in the largest PPROM randomized controlled trials that showed
a decrease in both maternal and neonatal morbidity): (1) ampicillin 2 g IV every 6 h and erythromycin 250 mg IV every 6 h for 48 h, followed by amoxicillin 250 mg PO every 8 h and erythromycin 333 mg PO every 8 h for 5 days (I-A); (2) erythromycin 250 mg PO every 6 h for 10 d (I-A)
7. Amoxicillin/clavulanicacidshouldnotbeused because of an increased risk of necrotizing enterocolitis in neonates exposed to this antibiotic. Amoxicillin without clavulanic acid is safe. (I-A)
8. WomenpresentingwithPPROMshould be screened for urinary tract infections, sexually transmitted infections, and group B Streptococcus carriage, and treated with appropriate antibiotics if positive. (II-2B)
*Evidence was approved by the Maternal Fetal Medicine Committee and Infectious Disease Committee of the Society of Obstetricians and Gynecologists of Canada
Etiology
• mostcasesidiopathic
• anencephalicfetuswithnopituitarygland
• placentalsulfatasedeficiency(X-linkedrecessiveconditionin1/2,000-1/6,000infants)–rare
Management (for singleton, cephalic fetus, otherwise uncomplicated)
• GA39wkwithadvancedmaternalage(>35yo):considerationshouldbegiventoIOLduetoincreased risk of stillbirth
• GA40-41wk:expectantmanagement
■ no evidence to support IOL or C/S unless other risk factors for morbidity are present (see prognosis)
• GA>41wk:offerIOLifvaginaldeliveryisnotcontraindicated
■ IOL shown to decrease C/S, fetal heart rate changes, meconium staining, macrosomia, and death
when compared with expectant management
• GA>41wkandexpectantmanagementelected:serialfetalsurveillance
■ fetal movement count by the mother
■ BPPq3-4d
• ifAFIisdecreased,labourshouldbeinduced
Prognosis
• if >42 wk, perinatal mortality 2-3x higher (due to progressive uteroplacental insufficiency)
• with increasing GA, higher rates of: intrauterine infection, asphyxia, meconium aspiration syndrome, placental insufficiency, placental aging and infarction, macrosomia, dystocia, fetal distress, operative
deliveries, pneumonia, seizures, and requirement of NICU admission, stillbirth
• morbidityincreasedwithHTNinpregnancy,DM,abruption,IUGR,andmultiplegestation
Degree of Prematurity
<24 wk 24-25 wk 26-34 wk 34-36 wk ≥37 wk
Prognosis
Management
Counsel regarding poor outcome due to pulmonary hypoplasia and offer option of pregnancy termination Individual consideration with counselling of parents regarding risks to preterm infants
Expectant management as prematurity complications are significant
“Grey zone” where risk of death from RDS and neonatal sepsis is the same
Induction of labour since the risk of death from sepsis is greater than RDS
• varies with gestational age
• 90%ofwomenwithPROMat28-34wkGAgointospontaneouslabourwithin1wk
• 50%ofwomenwithPROMat<26wkGAgointospontaneouslabourwithin1wk
• complications: cord prolapse, intrauterine infection (chorioamnionitis), premature delivery, limb
contracture, and pulmonary hypoplasia especially at very early gestation
Postterm Pregnancy
Definition
• pregnancy>42wkGA
Epidemiology
• 41wkGA:upto27% • >42wkGA:5.5%