Page 847 - TNFlipTest
P. 847
Toronto Notes 2019
Antepartum Care
Obstetrics OB7
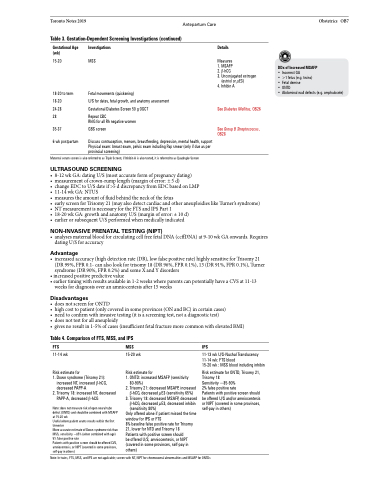
Table 3. Gestation-Dependent Screening Investigations (continued)
Gestational Age (wk)
15-20
18-20 to term 18-20
24-28
28
35-37
6 wk postpartum
Investigations
MSS
Fetal movements (quickening)
U/S for dates, fetal growth, and anatomy assessment
Gestational Diabetes Screen 50 g OGCT
Repeat CBC
RhIG for all Rh negative women
GBS screen
Discuss contraception, menses, breastfeeding, depression, mental health, support Physical exam: breast exam, pelvic exam including Pap smear (only if due as per provincial screening)
Details
Measures
1. MSAFP
2. β-hCG
3. Unconjugated estrogen
(estriol or μE3) 4. Inhibin A
See Diabetes Mellitus, OB26 See Group B Streptococcus,
OB28
• 8-12wkGA:datingU/S(mostaccurateformofpregnancydating)
• measurementofcrown-rumplength(marginoferror:±5d)
• changeEDCtoU/Sdateif>5ddiscrepancyfromEDCbasedonLMP
• 11-14wkGA:NTUS
• measurestheamountoffluidbehindtheneckofthefetus
• earlyscreenforTrisomy21(mayalsodetectcardiacandotheraneuploidieslikeTurner’ssyndrome) • NTmeasurementisnecessaryfortheFTSandIPSPart1
• 18-20wkGA:growthandanatomyU/S(marginoferror:±10d)
• earlierorsubsequentU/Sperformedwhenmedicallyindicated
NON-INVASIVE PRENATAL TESTING (NIPT)
• analysesmaternalbloodforcirculatingcellfreefetalDNA(ccffDNA)at9-10wkGAonwards.Requires dating U/S for accuracy
Advantage
• increasedaccuracy(highdetectionrate(DR),lowfalsepositiverate)highlysensitiveforTrisomy21 (DR 99%, FPR 0.1- can also look for trisomy 18 (DR 96%, FPR 0.1%), 13 (DR 91%, FPR 0.1%), Turner syndrome (DR 90%, FPR 0.2%) and some X and Y disorders
• increased positive predictive value
• earlier timing with results available in 1-2 weeks where parents can potentially have a CVS at 11-13
weeks for diagnosis over an amniocentesis after 15 weeks
Disadvantages
• doesnotscreenforONTD
• highcosttopatient(onlycoveredinsomeprovinces(ONandBC)incertaincases)
• needtoconfirmwithinvasivetesting(itisascreeningtest,notadiagnostictest)
• doesnottestforallaneuploidy
• gives no result in 1-5% of cases (insufficient fetal fracture more common with elevated BMI)
DDx of Increased MSAFP
• Incorrect GA
• >1 fetus (e.g. twins)
• Fetal demise
• ONTD
• Abdominal wall defects (e.g. omphalocele)
Maternal serum screen is also referred to as Triple Screen; if Inhibin A is also tested, it is referred to as Quadruple Screen
ULTRASOUND SCREENING
Table 4. Comparison of FTS, MSS, and IPS
FTS
11-14 wk
Risk estimate for
1. Down syndrome (Trisomy 21):
increased NT, increased β-hCG,
decreased PAPP-A
2. Trisomy 18: increased NT, decreased
PAPP-A, decreased β-hCG
Note: does not measure risk of open neural tube defect (ONTD) and should be combined with MSAFP at 15-20 wk
Useful where patient wants results within the first trimester
More accurate estimate of Down syndrome risk than MSS, sensitivity ~85% (when combined with age) 5% false positive rate
Patients with positive screen should be offered CVS, amniocentesis, or NIPT (covered in some provinces, self-pay in others)
MSS
15-20 wk
Risk estimate for
1. ONTD: increased MSAFP (sensitivity
80-90%)
2. Trisomy 21: decreased MSAFP, increased
β-hCG, decreased μE3 (sensitivity 65%) 3. Trisomy 18: decreased MSAFP, decreased
β-hCG, decreased μE3, decreased inhibin
(sensitivity 80%)
Only offered alone if patient missed the time window for IPS or FTS
8% baseline false positive rate for Trisomy 21, lower for NTD and Trisomy 18
Patients with positive screen should
be offered U/S, amniocentesis, or NIPT (covered in some provinces, self-pay in others)
IPS
11-13 wk U/S-Nuchal Translucency 11-14 wk: FTS blood
15-20 wk : MSS blood including inhibin
Risk estimate for ONTD, Trisomy 21, Trisomy 18
Sensitivity ~85-90%
2% false positive rate
Patients with positive screen should be offered U/S and/or amniocentesis or NIPT (covered in some provinces, self-pay in others)
Note: In twins, FTS, MSS, and IPS are not applicable; screen with NT, NIPT for chromosomal abnormalities and MSAFP for ONTDs